Prevention is always a good idea, but especially when brain cells regulating appetite and satiety can be obliterated by excitotoxic free glutamate consumed by pregnant women. And for free-glutamate-induced obesity there is no cure.
1957
The year that mass produced free glutamate was first consumed by pregnant women, causing brain damage followed by irreversible obesity in their fetuses.
For men only
As a man you probably don’t think about obesity being caused by pregnant women eating quantities of free glutamate in processed food. But think again. Because that same free glutamate ingested by pregnant women also lies at the root of the world’s infertility crisis.
True, infertility has many causes. Failure to eat a healthy diet is one of them. Breathing in toxic chemicals is another. An accident could be the third. But when a pregnant woman delivers more glutamate to her child during pregnancy then needed for normal development, the Jekyll and Hyde amino acid L-glutamate will destroy the part of the brain that was designed to oversee reproductive function.
Let me save you the trouble of trying to disprove this claim. There are no data with which you can do that, first, because to date no one other than myself has considered that glutamate-induced brain damage plays a role in both the obesity epidemic and the infertility crisis. Second, studies that allege to have demonstrated that monosodium glutamate is “safe” are flawed to the point of being fraudulent — as in using excitotoxic amino acids, which produce adverse reactions identical to those caused by MSG, in placebos. It is the U.S. producer of the flavor-enhancer monosodium glutamate, not neuroscientists interested in the role of free glutamate in brain function, that have produced those badly flawed studies.
Should you have interest in reviewing data on the subject you’ll find it summarized in “Getting to the root of obesity”and spelled out in detail in “Glutamic acid: the Jekyll and Hyde molecule behind the obesity epidemic.”
And don’t be fooled by the titles of those papers. Both infertility and obesity are caused by glutamate-induced brain damage done to the vulnerable brains of fetuses and newborns. The mechanisms are identical.
Adrienne Samuels
Resources
Review of animal data offered inappropriately as evidence that MSG is harmless
https://www.truthinlabeling.org/assets/seven_lines/Seven_Lines_Lines3.pdf
“Getting to the root of obesity”
https://www.truthinlabeling.org/assets/MASTERS_Perspective.pdf
“Glutamic acid: the Jekyll and Hyde molecule behind the obesity epidemic” https://www.truthinlabeling.org/assets/Masters_obesity_review.pdf
You could blame it on your mother, but there was no way for her to know
Did you know that obesity can be caused by pregnant women passing manufactured free glutamate to fetuses and newborns where it causes brain damage that in turn causes gross obesity, behavior disorders and reproductive disfunction (infertility)? Where do you find manufactured free glutamate? Think hydrolyzed proteins and MSG.
Watch for it.
Over the course of the next few blogs the Truth in Labeling Campaign will be unveiling the Seven Lines of Evidence that lead inevitably to the conclusion that manufactured free glutamate (MfG), such as that found in hydrolyzed proteins and monosodium glutamate (MSG) is a well-disguised poison – a poison that may well be hidden in your very own pantry.
The first blog in the series will be August 24.
_________________________________________
If you have questions or comments, we’d love to hear from you. If you have hints for others on how to avoid exposure to MfG, send them along, too, and we’ll put them up on Facebook. Or you can reach us at questionsaboutmsg@gmail.com and follow us on Twitter @truthlabeling.
Infertility? You could blame it on your mother – but there really was no way for her to have known.
According to the American Pregnancy Association, there are three main causes of infertility in males: a hypothalamic or pituitary disorder (1-2%), gonad disorder (30-40%), and sperm transport disorder (10-20%). That leaves 40-50% of cases with unknown causes.
None of these, however, is a root cause of infertility. They are names of categories of disorders that define infertility. Infertility may be traced back to a hypothalamic or pituitary disorder, for example, but the question remains –what caused those disorders to begin with?
Science combined with simple logic focused on problem solving says that hypothalamic, pituitary, gonad and sperm transport disorders are caused by damage done to the vulnerable, developing brains of fetuses and infants by brain-damaging chemicals, delivered by pregnant and lactating women.
1) Brain damage, followed by reproductive disorders, can be produced in human fetuses and newborns whose brains are not fully developed.
2) Excitotoxic amino acids (glutamic acid and aspartic acid) will cause brain damage when delivered in quantity to developing, vulnerable brains.
3) Brain-damaging amino acids consumed by pregnant and lactating women will be passed to their fetus through the placenta and to infants through mother’s milk.
4) Excitotoxic amino acids are readily available in processed and ultra-processed foods, protein powders and protein drinks, protein substitutes, flavor enhancers, pharmaceuticals, dietary supplements, cosmetics, and vaccine excipients.
Here’s how it works
A study demonstrating glutamate-induced brain damage was published in Science by John Olney, M.D. way back in 1969, titled “Brain lesions, obesity, and other disturbances in mice treated with monosodium glutamate.” Olney established that:
1) Brain damage, followed by reproductive disorders, can be produced in newborn mice, whose brains are not fully developed. A student in Olney’s lab had observed that mice being used in studies of glutamate-induced retinal dysfunction had become grotesquely obese. A series of studies by Olney and others followed. Many of them were studies of MSG fed to animals.
2) Excitotoxic amino acids (glutamic acid and aspartic acid) will cause brain damage when delivered in quantity to the vulnerable brains of neonatal mice.
When present in amounts needed for normal body function, glutamic acid is essential. But when accumulated in amounts greater than that needed for normal body function, the neurotransmitter glutamic acid becomes an excitotoxic neurotransmitter, firing repeatedly, damaging the cells that host targeted glutamate-receptors and/or causing death by over-exciting those glutamate receptors until their host cells die.
3) Excitotoxic amino acids can be delivered to neonatal mice through feeding.
In the laboratory, researchers manipulated dosage of glutamic acid and aspartic acid until they found those that were lethal to brain cells.
Additional confirmation of the brain-damaging effects of excitotoxic free glutamic acid comes from research focused on identifying and understanding human diseases and abnormalities associated with glutamate, often for the purpose of finding drugs that would mitigate glutamate’s adverse effects. By 1980, glutamate-associated disorders such as headaches, asthma, diabetes, muscle pain, atrial fibrillation, ischemia, trauma, seizures, stroke, Alzheimer’s disease, amyotrophic lateral sclerosis (ALS), Huntington’s disease, Parkinson’s disease, depression, multiple sclerosis, schizophrenia, obsessive-compulsive disorder (OCD), epilepsy, addiction, attention-deficit/hyperactivity disorder (ADHD), frontotemporal dementia and autism were on the rise, and evidence of the brain-damaging effects of glutamate were generally accepted by the scientific community.
Having provided evidence that brain lesions can be induced in fetuses and neonates thru the introduction of excitotoxins, and having pointed out that glutamic acid is an excitotoxin, the only question that remains is how excitotoxic glutamic acid could get to the vulnerable brain of the infant or the fetus causing brain damage, destroying those areas of the arcuate nucleus that would regulate reproductive function had they not been obliterated.
To be excitotoxic, glutamic acid has to be accumulated in considerable quantity. There have always been excitotoxins, although not in food in excessive amounts. But that changed in 1957 when there was a transformation in the method of producing the glutamate used in MSG from extraction of glutamate from a protein source, which had been a slow and costly method, to using carefully selected genetically modified bacteria to excrete glutamate through their cell walls. That allowed virtually unlimited production of manufactured free glutamate and MSG.
It wasn’t long before food manufacturers found that profits could be increased by using manufactured free glutamate to produce their own flavor-enhancing additives, and dozens of excitotoxic ingredients were added to the food supply. Over the next two decades, the marketplace became flooded with manufactured/processed free glutamate in ingredients such as hydrolyzed proteins, yeast extracts, maltodextrin, soy protein isolate and MSG — and the large amounts of manufactured free glutamate needed to cause excitotoxicity became readily available to anyone consuming a number of processed food products during the course of a day.
Today, there is more than sufficient excitotoxic glutamic acid in food, “fake” food and dietary supplements to cause excitotoxicity.
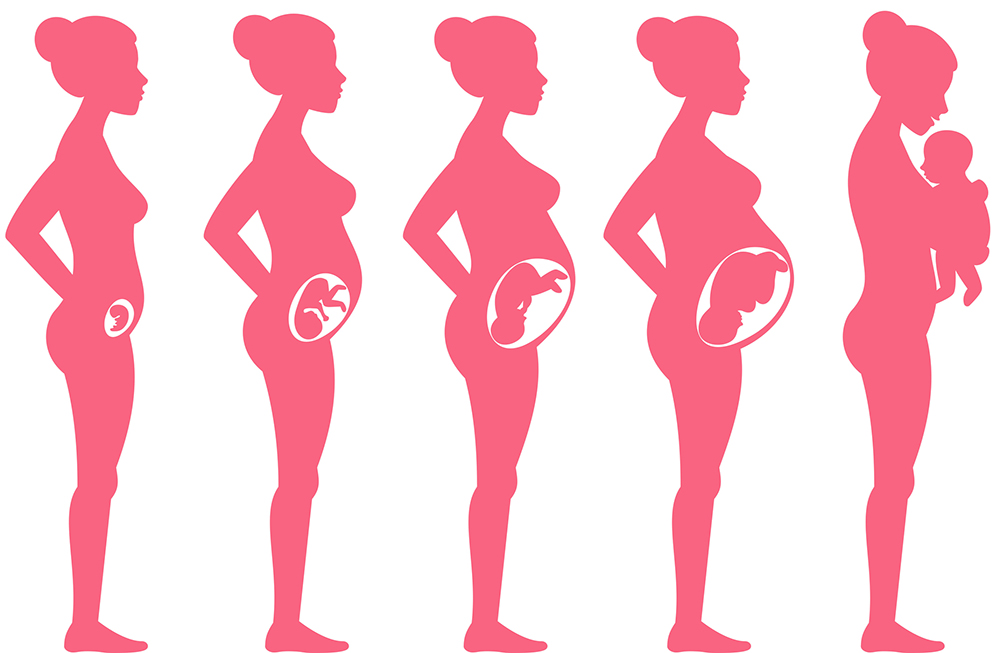
Once it is understood that excitotoxins are readily available, transport to fetus and newborn becomes easy to understand. Nourishment (and not so nourishing material) is delivered to the fetus in the form of material ingested by a pregnant woman and passed to the fetus through the placenta.
Data confirm that free glutamate can be passed in excessive quantities to neonates and fetuses by expectant mothers who ingest excessive amounts. Glutamate can cross the placenta during pregnancy, can cross the blood brain barrier (BBB) in an unregulated manner during development and can pass through the five circumventricular organs (unique areas of the brain that lie outside the BBB) which are leaky at best at any stage of life. Moreover, the BBB is easily damaged by fever, stroke, trauma to the head, seizures, ingestion of MSG, and the normal process of aging. Similar to drugs and alcohol, free glutamate can also be passed to infants through mothers’ milk.
But a crisis? All of a sudden?
There has always been infertility, but not in such numbers that it could be called a crisis. There have always been amino acids that could become excitotoxic, but not to the extent that they could accumulate and become excitotoxic. The infertility crisis began after amino acids with excitotoxic potential became available in the quantity necessary to cause them to become excitotoxic – made possible by the 1957 introduction of monosodium glutamate produced by bacterial fermentation.
Science combined with a good dose of logic tell us that glutamic acid passed to fetus and neonate by pregnant and lactating women is the root cause of the infertility crisis.
If you have questions or comments, we’d love to hear from you. If you have hints for others on how to avoid exposure to MfG, send them along, too, and we’ll put them up on Facebook. Or you can reach us at questionsaboutmsg@gmail.com and follow us on Twitter @truthlabeling.
Resources
American Pregnancy Association https://americanpregnancy.org/getting-pregnant/male-infertility/
Olney JW. Brain lesions, obesity, and other disturbances in mice treated with monosodium glutamate. Science. 1969;164(880):719-721.
Olney JW. Glutamate-induced neuronal necrosis in the infant mouse hypothalamus. J Neuropathol Exp Neurol. 1971;30(1):75-90.
Burde RM, Schainker B, Kayes J. Acute effect of oral and subcutaneous administration of monosodium glutamate on the arcuate nucleus of the hypothalamus in mice and rats. Nature. 1971;233(5314):58-60.
Olney JW, Sharpe LG, Feigin RD. Glutamate-induced brain damage in infant primates. J Neuropathol Exp Neurol. 1972;31(3):464-488.
Burde RM, Schainker B, Kayes J. Monosodium glutamate: necrosis of hypothalamic neurons in infant rats and mice following either oral or subcutaneous administration. J Neuropathol Exp Neurol. 1972;31(1):181.
Olney JW, Rhee V, DeGubareff T. Neurotoxic effects of glutamate on mouse area postrema. Brain Res. 1977;120(1):151-157.
Olney JW, Ho OL. Brain damage in infant mice following oral intake of glutamate, aspartate or cystine. Nature. 1970;227:609-611.
Lemkey-Johnston N, Reynolds WA. Nature and extent of brain lesions in mice related to ingestion of monosodium glutamate: a light and electron microscope study. J Neuropath Exp Neurol. 1974;33(1):74-97.
Takasaki, Y. Protective effect of mono- and disaccharides on glutamate-induced brain damage in mice. Toxicol Lett. 1979;4(3): 205-210.
Takasaki, Y. Protective effect of arginine, leucine, and preinjection of insulin on glutamate neurotoxicity in mice. Toxicol Lett. 1980;5(1):39-44.
Lemkey-Johnston, N, Reynolds WA. Nature and extent of brain lesions in mice related to ingestion of monosodium glutamate: a light and electron microscope study. J Neuropath Exp Neurol. 1974;33(1):74-97.
Bahadoran Z, Mirmiran P, Ghasemi A. Monosodium Glutamate (MSG)-Induced Animal Model of Type 2 Diabetes. Methods Mol Biol. 2019;1916:49-65.
Sharma A. Monosodium glutamate-induced oxidative kidney damage and possible mechanisms: a mini-review. J Biomed Sci. 2015;22:22:93.
Kurose T, Sugano E, Sugai A, Shiraiwa R, Kato M, Mitsuguchi Y, Takai Y, Tabata K, Honma Y, Tomita H. Neuroprotective effect of a dietary supplement against glutamate-induced excitotoxicity in retina. Int J Ophthalmol. 2019;12(8):1231-1237.
Moneret-Vautrin DA. Monosodium glutamate-induced asthma: study of the potential risk of 30 asthmatics and review of the literature. Allerg Immunol (Paris). 987;19(1):29-35.
Olloquequi J, Cornejo-Córdova E, Verdaguer E, Soriano FX, Binvignat O, Auladell C, Camins A. Excitotoxicity in the pathogenesis of neurological and psychiatric disorders: Therapeutic implications. J Psychopharmacol. 2018;32(3):265-275.
Binvignat O, Olloquequi J. Excitotoxicity as a Target against Neurodegenerative Processes. Curr Pharm Des. 2020 Jan 13. doi:10.2174/1381612826666200113162641.
Hashimoto S. Discovery and History of Amino Acid Fermentation.
Adv Biochem Eng Biotechnol. 2017;159:15-34.
Sano C. History of glutamate production. Am J Clin Nutr. 2009;90(3):728S-732S.
Frieder B, Grimm VE. Prenatal monosodium glutamate (MSG) treatment given through the mother’s diet causes behavioral deficits in rat offspring. Intern J Neurosci. 1984;23(2):117-126.
Gao J, Wu J, Zhao XN, Zhang WN, Zhang YY, Zhang ZX. [Transplacental neurotoxic effects of monosodium glutamate on structures and functions of specific brain areas of filial mice.] Sheng Li Hsueh Pao Acta Physiologica Sinica. 1994;46(1):44-51.
Yu T, Zhao Y, Shi W, Ma R, Yu L. Effects of maternal oral administration of monosodium glutamate at a late stage of pregnancy on developing mouse fetal brain. Brain Res. 1997;747(2):195-206.
Arya V, Demarco VG, Issar M, Hochhaus G. Contrary to adult, neonatal rats show pronounced brain uptake of corticosteroids.
Drug Metab Dispos. 2006;34(6):939-42.
Moretti R, Pansiot J, Bettati D, Strazielle N, Ghersi-Egea JF, Damante G, Fleiss B, Titomanlio L, Gressens P. Blood-brain barrier dysfunction in disorders of the developing brain. Front Neurosci. 2015 Feb 17;9:40.
Price MT, Olney JW, Lowry OH, Buchsbaum S. Uptake of exogenous glutamate and aspartate by circumventricular organs but not other regions of brain. J Neurochem. 1981;36(5):1774-1780.
Skultetyova I, Tokarev D, Jezova D. Stress-induced increase in blood-brain barrier permeability in control and monosodium glutamate-treated rats. Brain Res Bull. 1998;45(2):175-178.
Broadwell RD, Sofroniew MV. Serum proteins bypass the blood-brain fluid barriers for extracellular entry to the central nervous system. Exp Neurol. 1993;120(2):245-263.
Blaylock RL. Excitotoxins: The Taste That Kills. Santa Fe, New Mexico: Health Press; 1994.
Nemeroff CB, Crisley FD. Monosodium L-glutamate induced convulsions: temporary alteration in blood-brain barrier permeability to plasma proteins. Environ Physiol Biochem. 1975;5(6):389-395.
Brown RA, Dakkak H, Seabrook JA. Is Breast Best? Examining the effects of alcohol and cannabis use during lactation. J Neonatal Perinatal Med. 2018;11(4):345-356.